************************************************
What Are Prenatal Screening Tests?
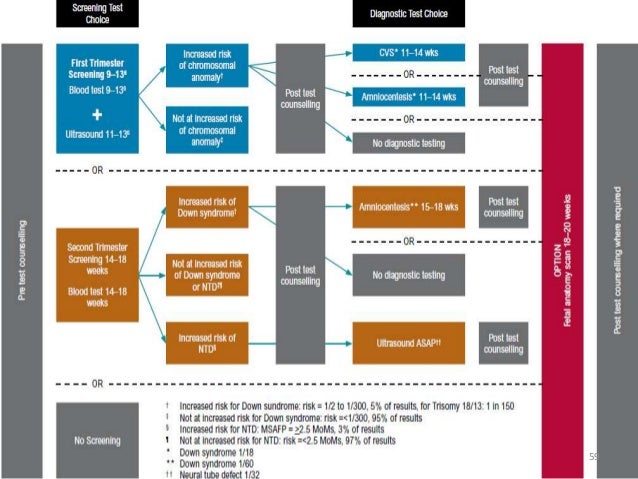
Prenatal screening tests are a set of procedures that are performed during pregnancy on expectant mothers to determine whether a baby is likely to have specific birth defects. Most of these tests are noninvasive. They’re usually performed during the first and second trimesters, although some are performed during the third.
A screening test can only provide your risk, or probability, that a particular condition exists. When the results of a screening test are positive, diagnostic tests can provide a definitive answer.
Some prenatal screening tests are routine procedures, such as glucose tolerance tests, which check for gestational diabetes. Women who have a higher risk of having a child with certain conditions are usually offered additional screening tests. For example, pregnant women who’ve lived in regions where tuberculosis is common should have a tuberculin skin test.
When Are Prenatal Screening Tests Done?
First trimester screening tests can begin as early as 10 weeks. These usually involve blood tests and an ultrasound. They test your baby’s overall development and check to see if your baby is at risk for genetic conditions, such as Down syndrome. They also check your baby for heart defects, cystic fibrosis, and other developmental problems.
Second trimester screening tests occur between 14 and 18 weeks. They can involve a blood test, which tests whether a mother is at risk for having a child with Down syndrome or neural tube defects, as well as an ultrasound.
First Trimester Screening Tests
Ultrasound
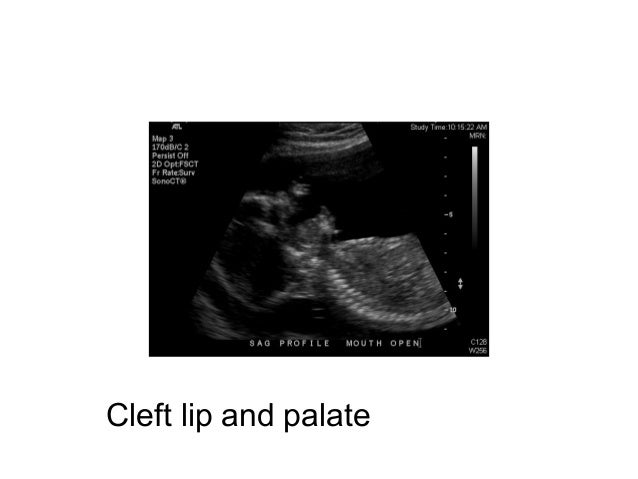
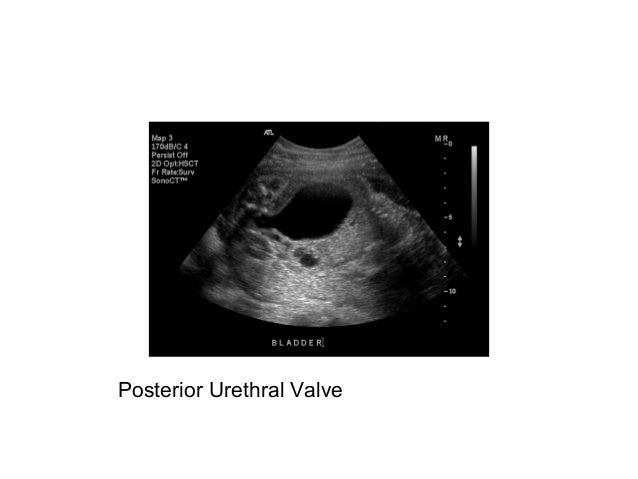
An ultrasound uses sound waves to create an image of the baby in the uterus. The test is used to determine the size and position of your baby, confirm how far along you are in your pregnancy, and find any potential abnormalities in the structure of your baby’s growing bones and organs.
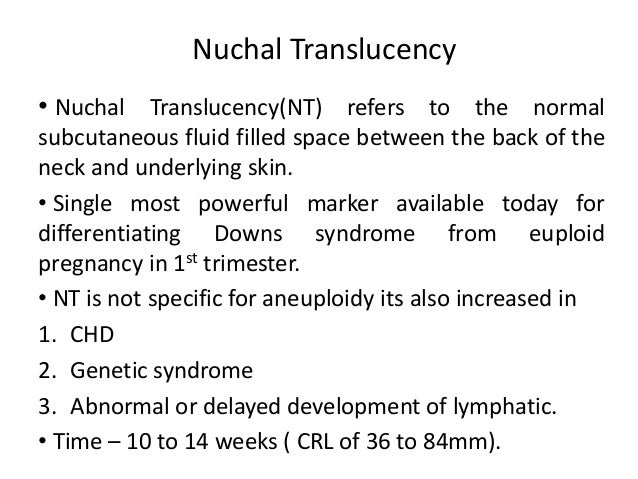
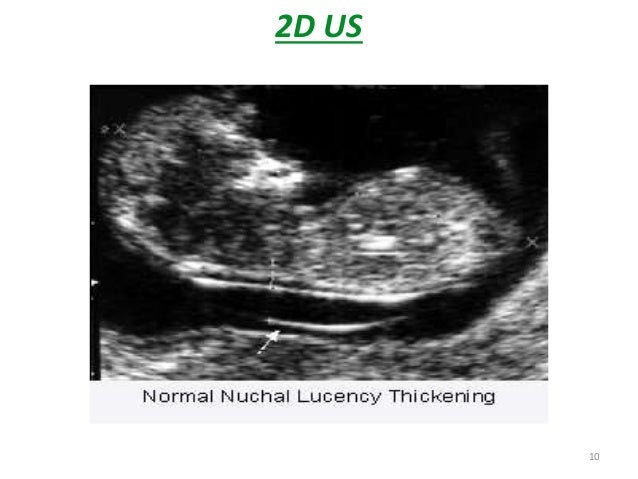
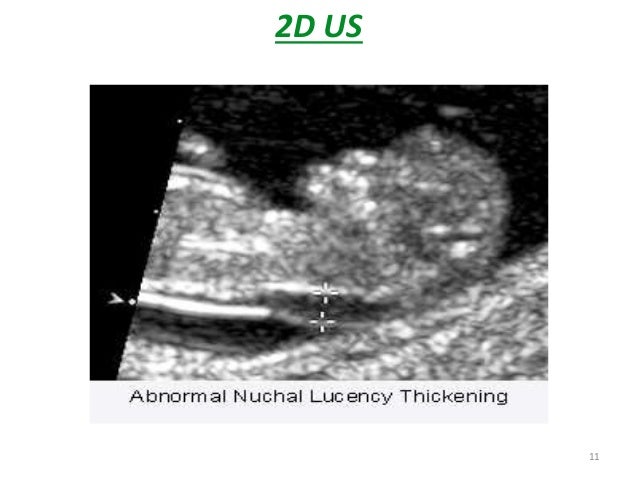
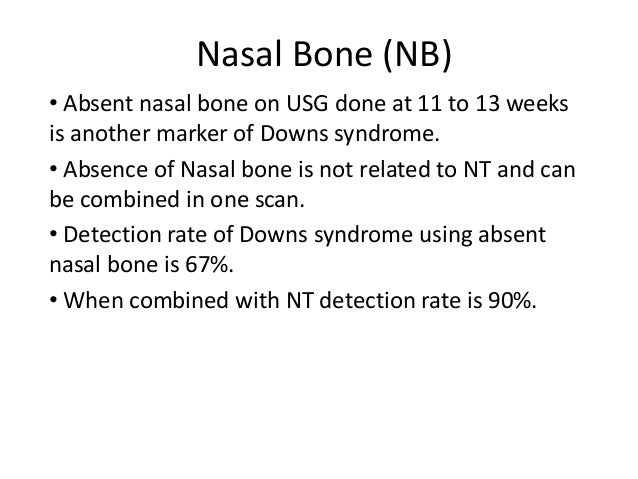
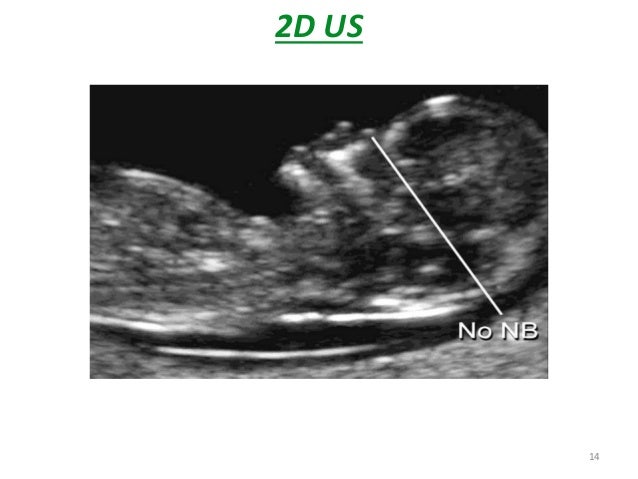
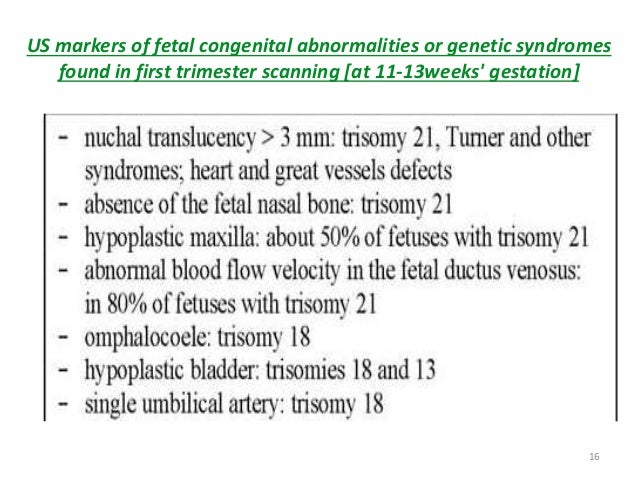
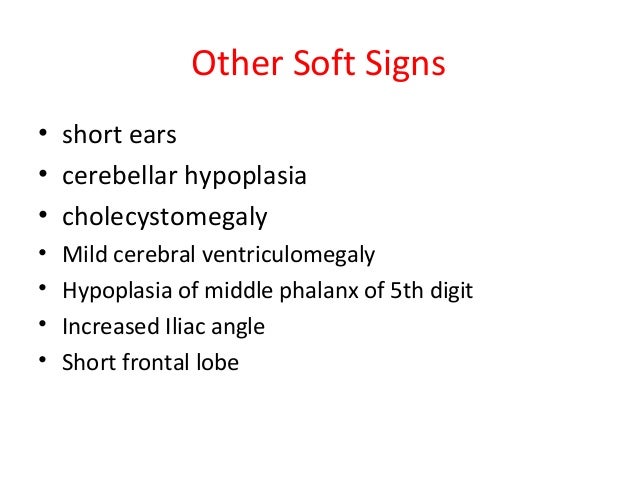
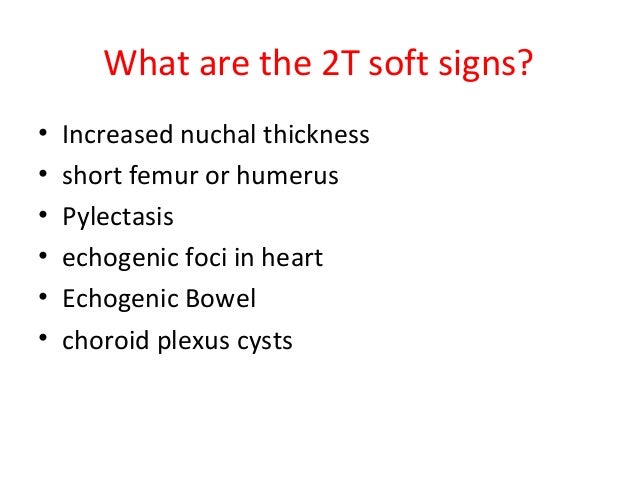
A special ultrasound called a nuchal translucency ultrasound is performed between the 11th and 14th weeks of pregnancy. This ultrasound checks the accumulation of fluid at the back of your baby’s neck. When there’s more fluid than normal, this means there’s a higher risk of Down syndrome.
During the second trimester, a more detailed ultrasound, which is often called a fetal anatomy survey, is used to evaluate the baby carefully from head to toe for any birth defects. However, not all birth defects are visible by ultrasound.
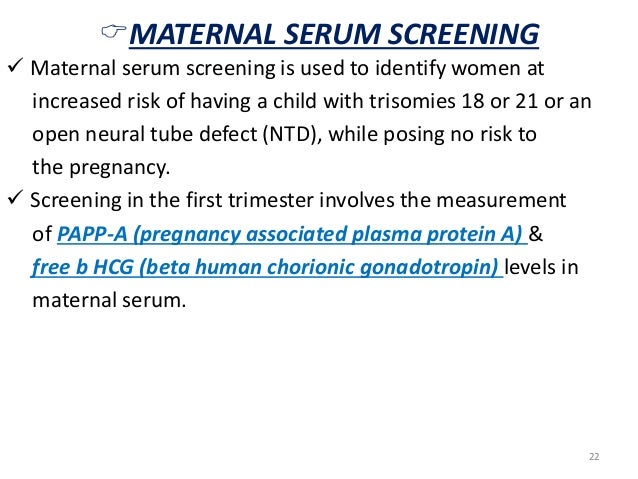
Early Blood Tests
During the first trimester, two types of blood tests called a sequential integrated screening test and a serum integrated screening are conducted. They’re used to measure the levels of certain substances in your blood, namely, pregnancy-associated plasma protein-A and a hormone called human chorionic gonadotropin. Abnormal levels of either mean there’s a higher risk of a chromosome abnormality.
At your first prenatal visit, your blood may also be tested to see if you’re immunized against rubella and to screen for syphilis, hepatitis B, and HIV.
A blood test will also be used to determine your blood type and Rh factor, which determines your Rh compatibility with your growing fetus. You can be either Rh-positive or Rh-negative. Most people are Rh-positive, but if a mother is found to be Rh-negative, her body will produce antibodies that will affect any subsequent pregnancies.
When there’s an Rh incompatibility, most women will be given a shot of Rh-immune globulin at 28 weeks and again a few days after delivery. Incompatibility occurs if a woman is Rh-negative and her baby is Rh-positive. If the woman is Rh-negative and her baby’s positive, she’ll need the shot. If her baby is Rh-negative, she won’t.
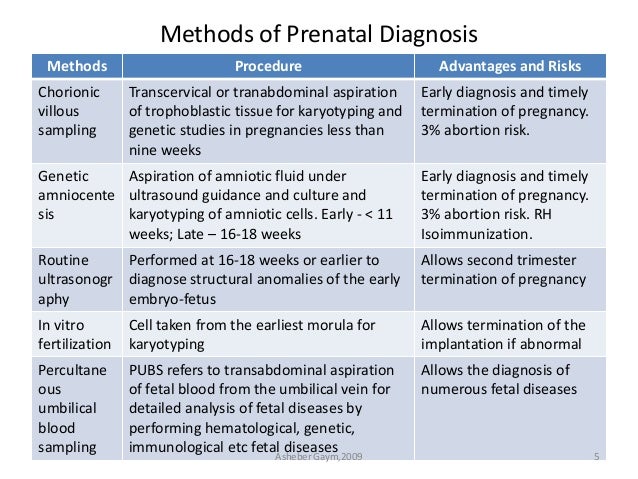
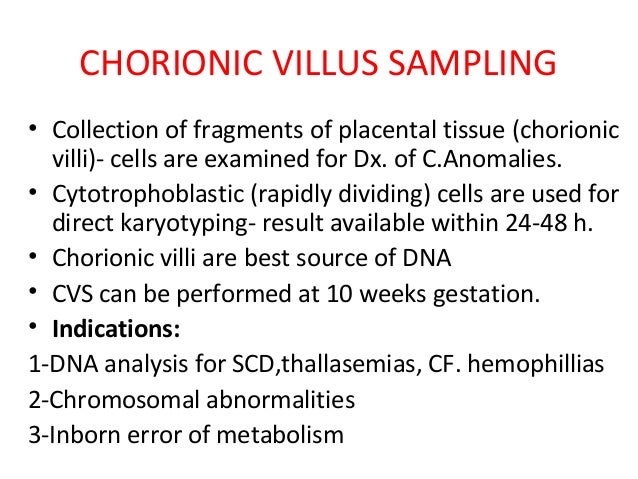
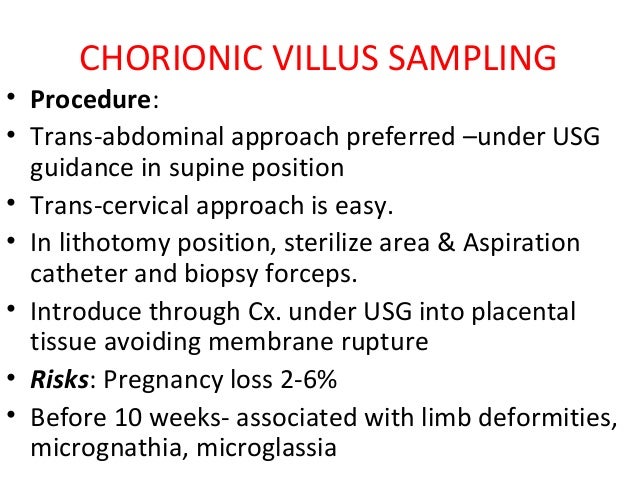
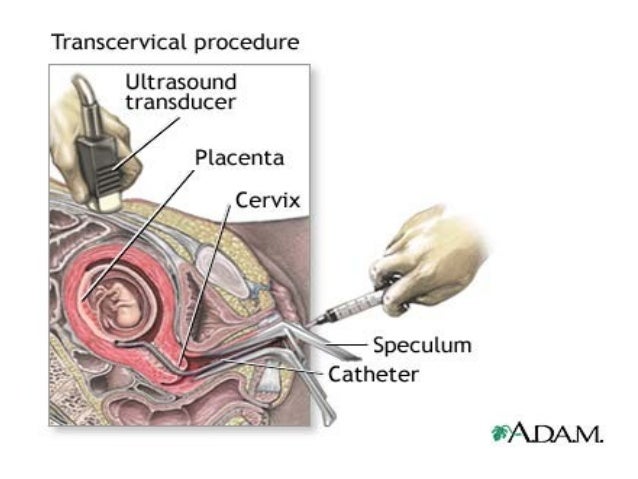
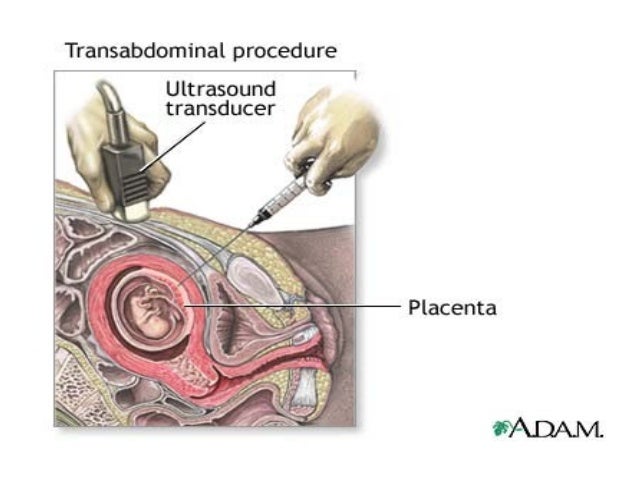
Chorionic Villus Sampling
Chorionic villus sampling is an invasive screening test that involves taking a small piece of tissue from the placenta. It’s usually performed between the 10th and 12th weeks and is used to test for genetic abnormalities, like Down syndrome, and birth defects. There are two types. One type tests through the belly, which is called a transabdominal test, and one type tests through the cervix, which is called a transcervical test.
Testing has some side effects, like cramps or spotting. There’s also a small risk of miscarriage.
Second Trimester Screening Tests
Blood Tests
A quad marker screening test is a blood test conducted during the second trimester. It’s done to test your blood for indications of birth defects, such as Down syndrome. It measures four of the fetal proteins.
A quad marker screening is typically offered if you start prenatal care too late to receive either the serum integrated screening or the sequential integrated screening. It has a lower detection rate for Down syndrome and other birth defects than a sequential integrated screening test or serum integrated screening test.
Glucose Screening
A glucose screening test checks for gestational diabetes. This is usually a condition that can develop during pregnancy. It’s usually temporary. Gestational diabetes can increase your potential need for a caesarean delivery because babies of mothers with gestational diabetes are usually born larger. Your child may also have low blood sugar in the days following delivery.
The test is usually performed during the second trimester. It involves drinking a sugary solution, having your blood drawn, and then checking your blood sugar levels. If you do test positive for gestational diabetes, you have a higher risk of developing diabetes within the following 10 years, and you should get the test again after the pregnancy.
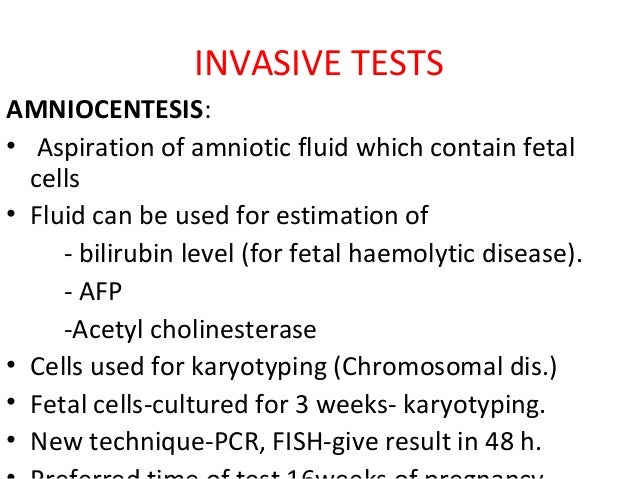
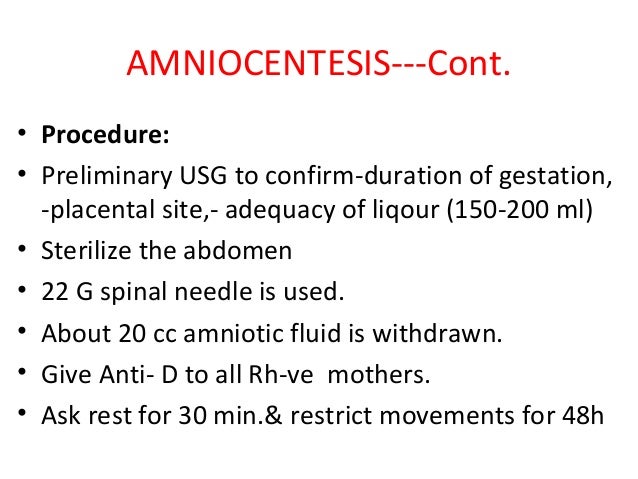
Amniocentesis
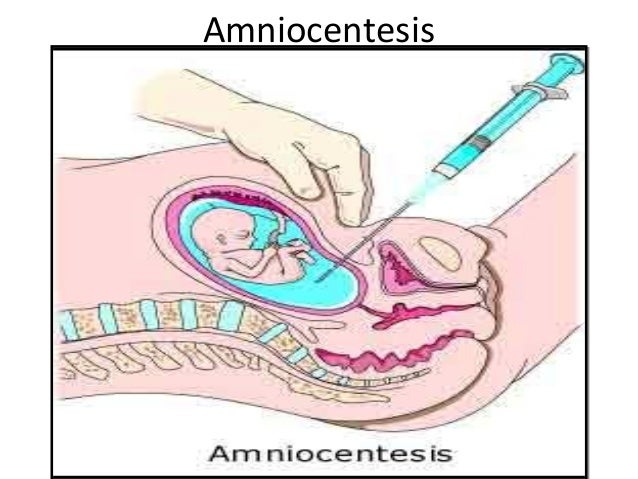
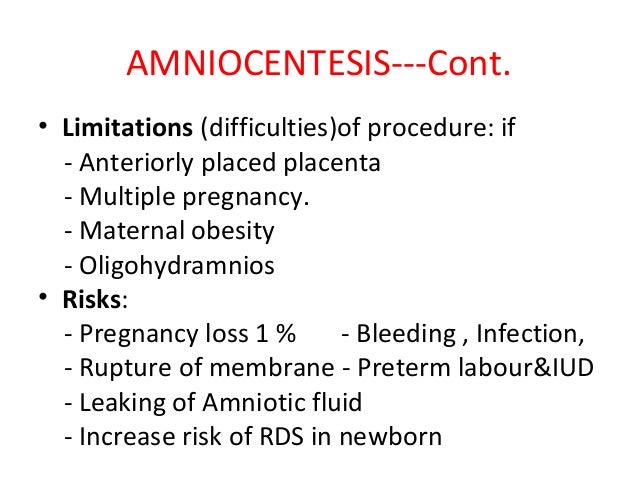
During amniocentesis, amniotic fluid is removed from the uterus for testing. Amniotic fluid surrounds the baby during pregnancy. It contains fetal cells with the same genetic makeup as the baby, as well as various chemicals produced by the baby’s body. There are several types of amniocentesis.
A genetic amniocentesis tests for genetic abnormalities, such as Down syndrome and spina bifida. A genetic amniocentesis is usually performed after week 15 of the pregnancy. It may be considered if:
- a prenatal screening test showed abnormal results
- you had a chromosomal abnormality during a previous pregnancy
- you’re 35 or older
- you have a family history of a specific genetic disorder
- you or your partner is a known carrier of a genetic disorder
A maturity amniocentesis is performed later, during the third trimester, to determine whether or not your baby’s lungs are ready for birth. This diagnostic test is only done if a planned early delivery through either induction of labor or a cesarean delivery is being considered for medical reasons. It’s usually done between weeks 32 and 39.
Third Trimester Screening Tests
Group B Strep Screening
Group B Streptococcus (GBS) is a type of bacteria that can cause serious infections in pregnant women and newborns. GBS is often found in the following areas in healthy women:
- the mouth
- the throat
- the lower intestinal tract
- the vagina
GBS in the vagina generally isn’t harmful to a woman regardless of whether she’s pregnant. However, it can be very harmful to a newborn baby who doesn’t yet have a robust immune system. GBS can cause serious infections in babies exposed during birth. You can be screened for GBS with a swab taken from your vagina and rectum at 35-37 weeks.
If you test positive for GBS, you’ll receive antibiotics while you’re in labor to reduce your baby’s risk of contracting a GBS infection.
Prenatal Diagnostic Tests
Diagnostic tests are the next step after a screening test that yields a positive result. They leave virtually no doubt as to the existence or absence of certain birth defects.
Diagnostic tests are more invasive than screening tests. They’re usually only done if there’s a specific concern, if a screening test indicates a problem, or if your age, family history, or medical history suggests that you may have an increased risk for a problematic pregnancy. Diagnostic tests can carry a very small risk of miscarriage.
*****************************************************************************
Prenatal diagnosis
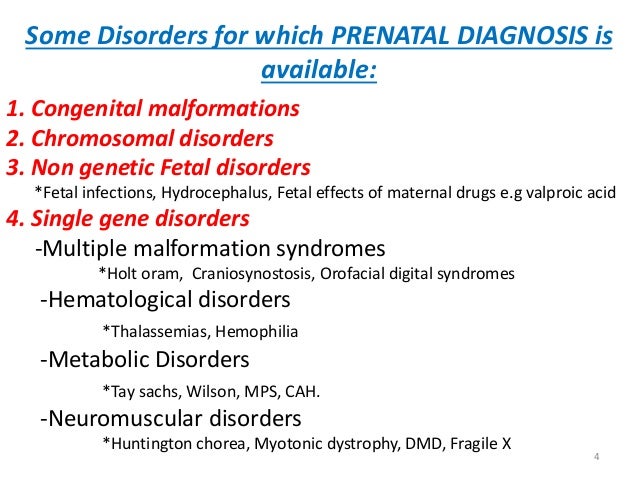
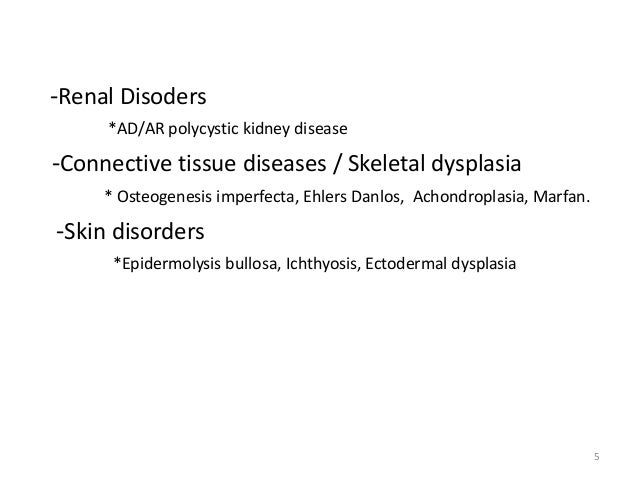
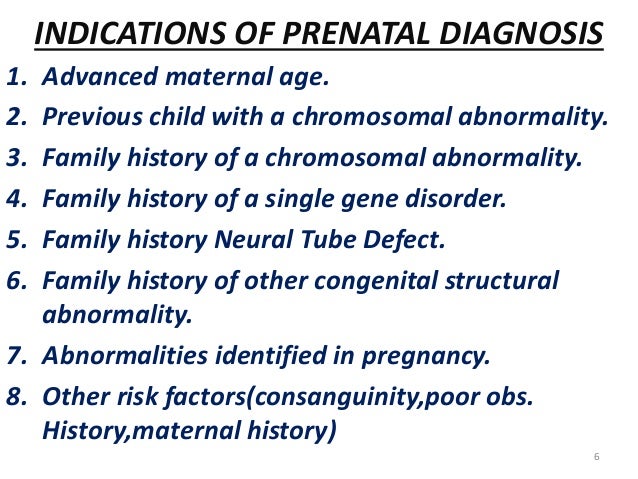
Prenatal diagnosis employs a variety of techniques to determine the health and condition of an unborn fetus. Without knowledge gained by prenatal diagnosis, there could be an untoward outcome for the fetus or the mother or both. congenital anomalies account for 20 to 25% of perinatal deaths. Specifically, prenatal diagnosis is helpful for:
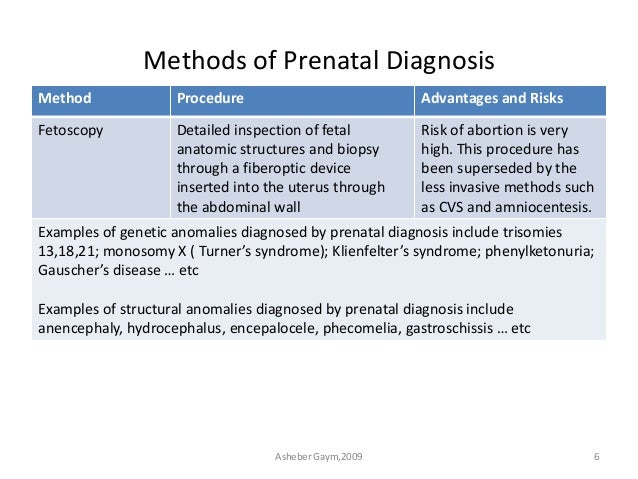
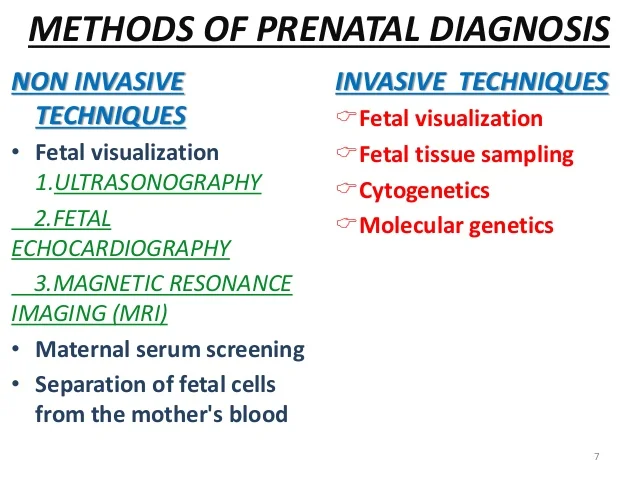
There are a variety of non-invasive and invasive techniques available for prenatal diagnosis. Each of them can be applied only during specific time periods during the pregnancy for greatest utility. The techniques employed for prenatal diagnosis include:
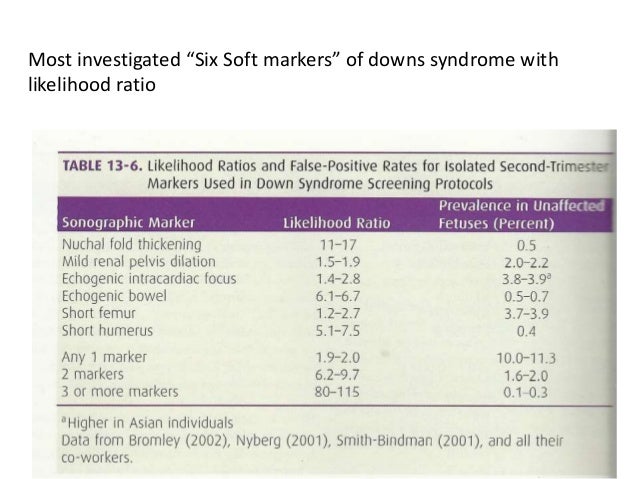
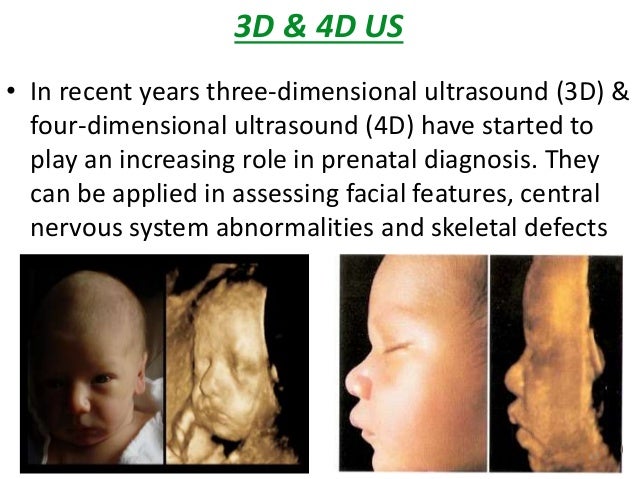
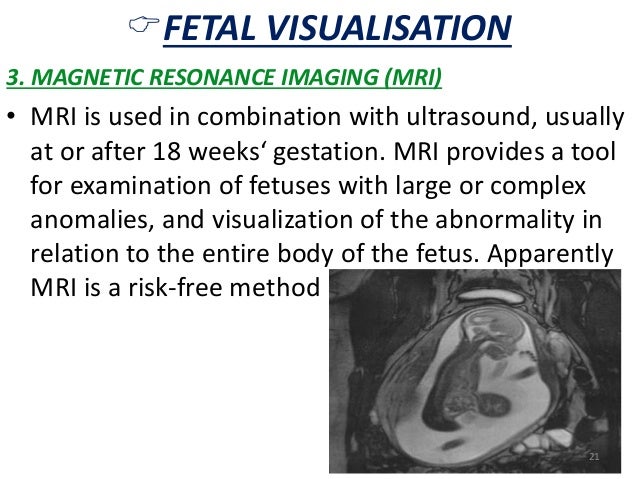
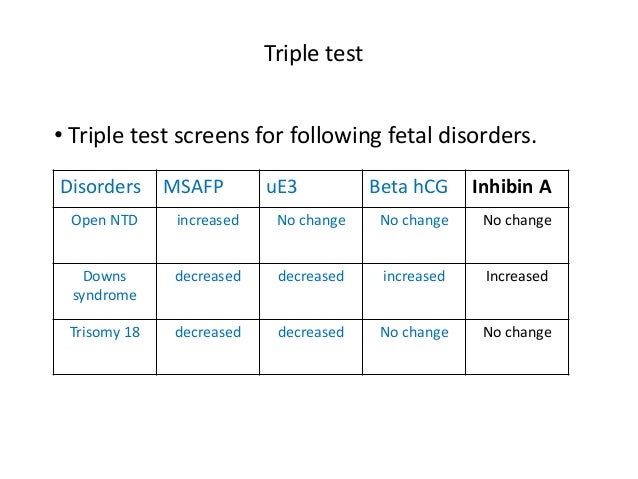
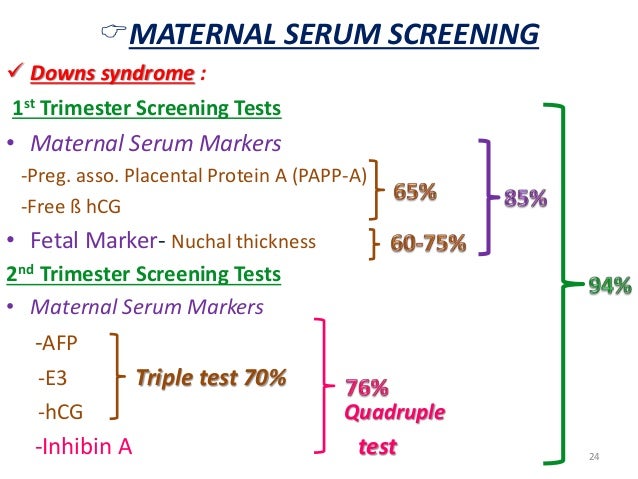
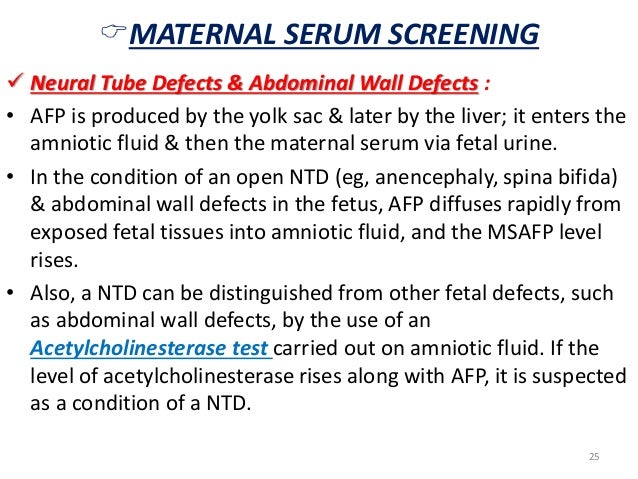
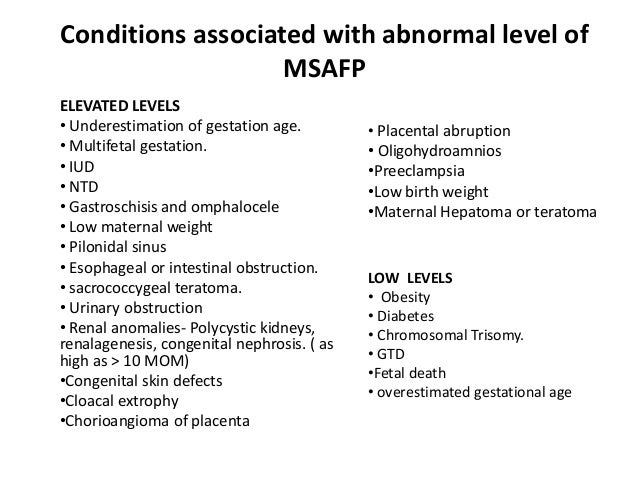
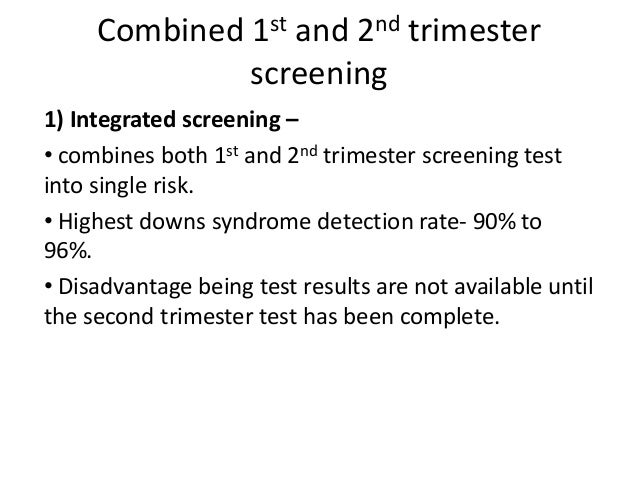
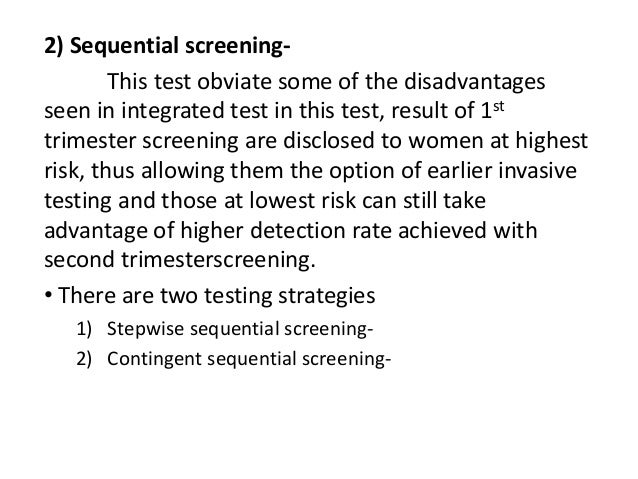
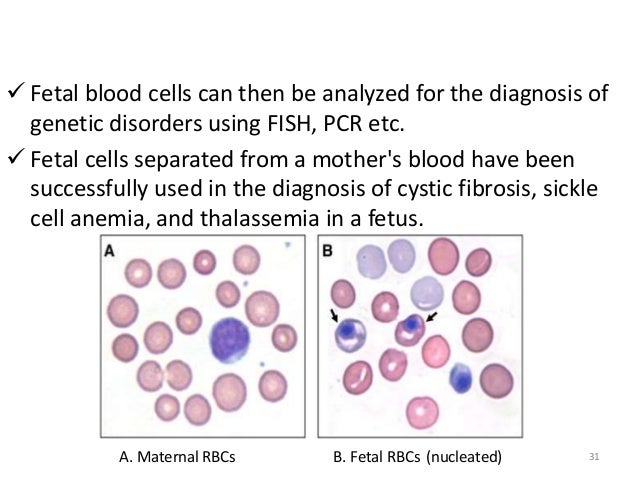
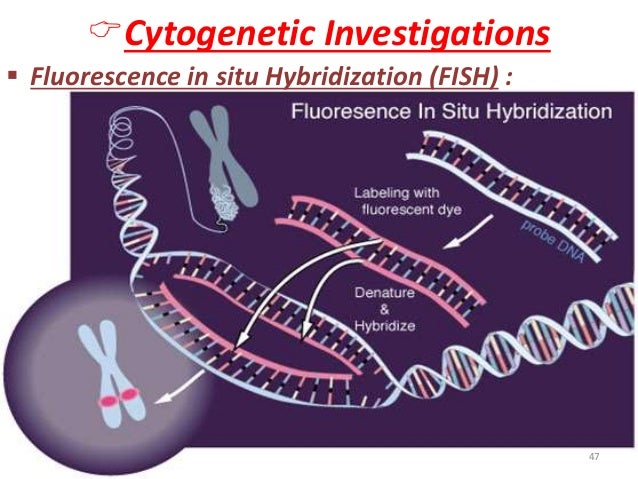
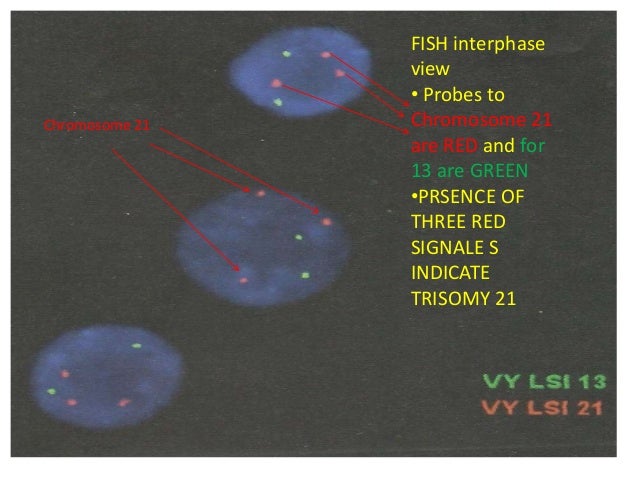
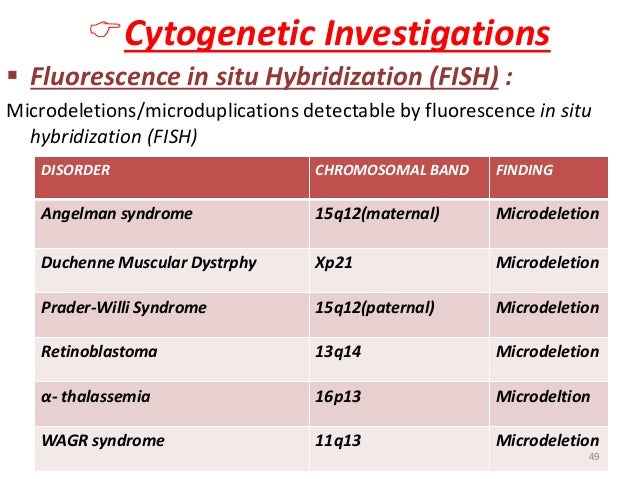
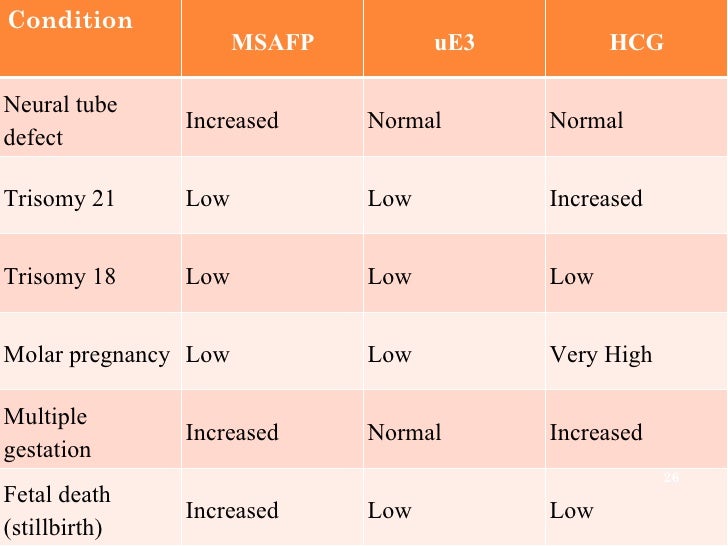
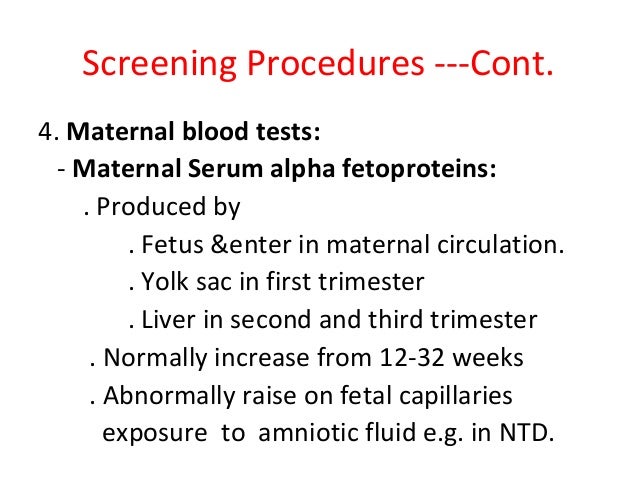
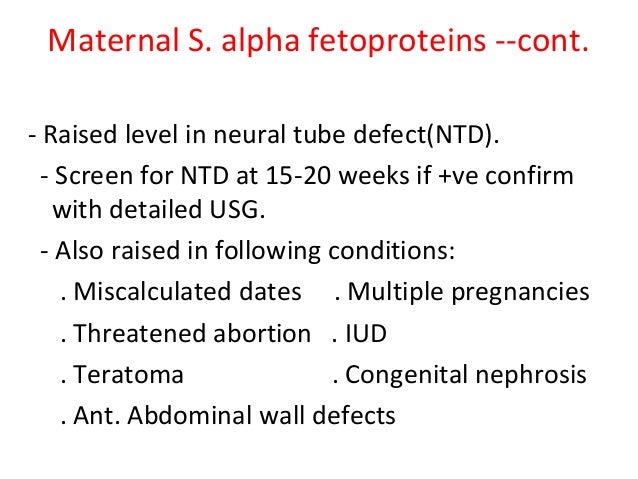
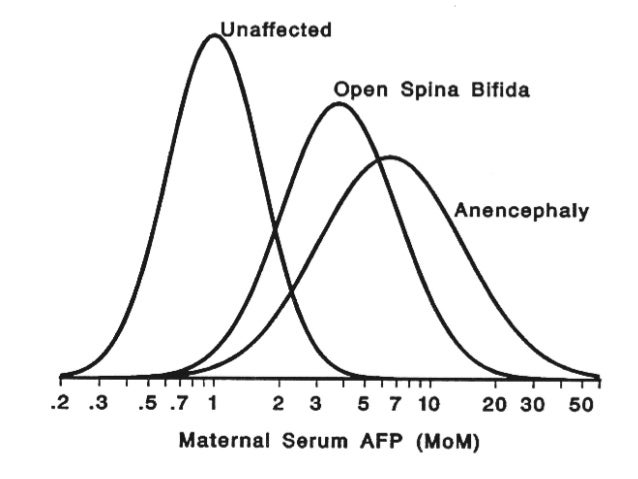
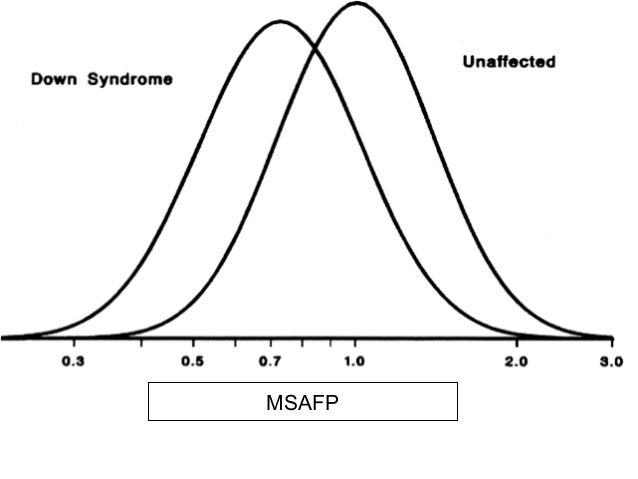
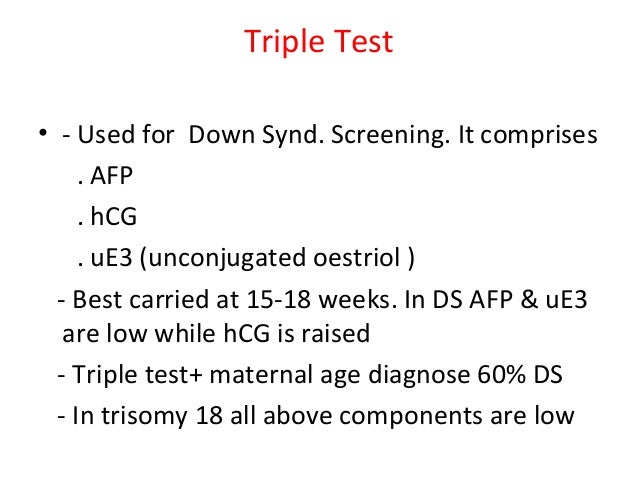
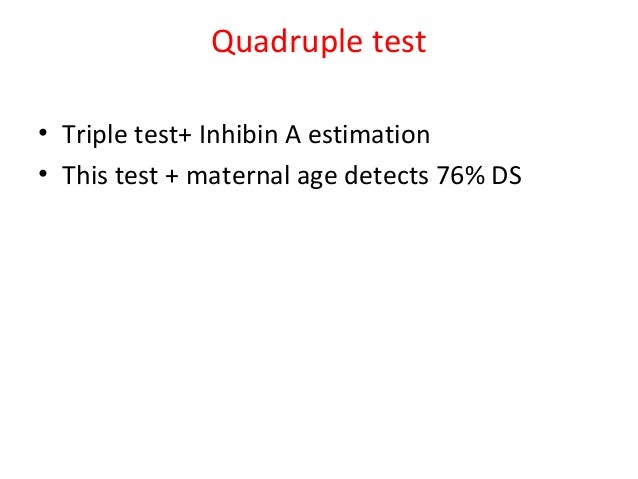
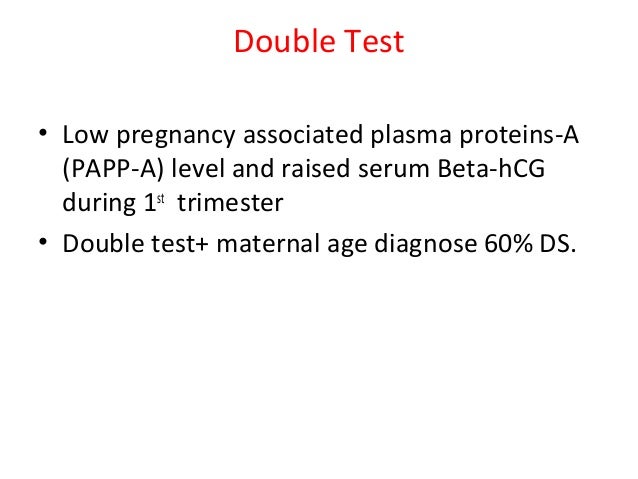
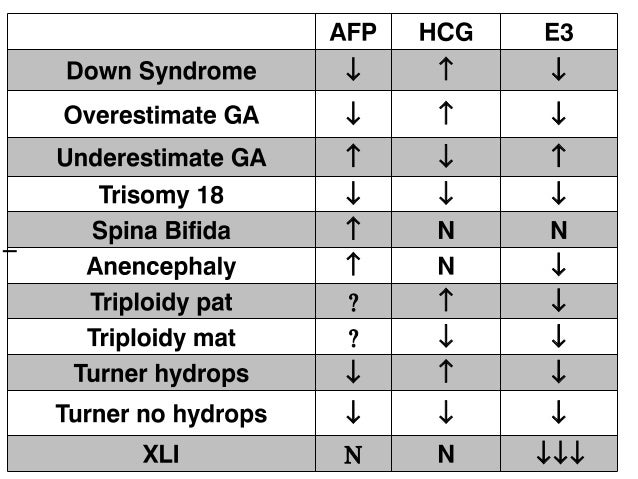
UltrasonographyThis is a non-invasive procedure that is harmless to both the fetus and the mother. High frequency sound waves are utilized to produce visible images from the pattern of the echos made by different tissues and organs, including the baby in the amniotic cavity. The developing embryo can first be visualized at about 6 weeks gestation. Recognition of the major internal organs and extremities to determine if any are abnormal can best be accomplished between 16 to 20 weeks gestation. Although an ultrasound examination can be quite useful to determine the size and position of the fetus, the size and position of the placenta, the amount of amniotic fluid, and the appearance of fetal anatomy, there are limitations to this procedure. Subtle abnormalities may not be detected until later in pregnancy, or may not be detected at all. A good example of this is Down syndrome (trisomy 21) where the morphologic abnormalities are often not marked, but only subtle, such as increased nuchal translucency (the subcutaneous space between skin surface and underlying cervical spine). AmniocentesisThis is an invasive procedure in which a needle is passed through the mother’s lower abdomen into the amniotic cavity inside the uterus. Enough amniotic fluid is present for this to be accomplished starting about 14 weeks gestation. For prenatal diagnosis, most amniocenteses are performed between 14 and 20 weeks gestation. However, an ultrasound examination always proceeds amniocentesis in order to determine gestational age, the position of the fetus and placenta, and determine if enough amniotic fluid is present. Within the amniotic fluid are fetal cells (mostly derived from fetal skin) which can be\ grown in culture for chromosome analysis, biochemical analysis, and molecular biologic analysis. In the third trimester of pregnancy, the amniotic fluid can be analyzed for determination of fetal lung maturity. This is important when the fetus is below 35 to 36 weeks gestation, because the lungs may not be mature enough to sustain life following birth. This is because the lungs are not producing enough surfactant. After birth, the infant could develop respiratory distress syndrome from hyaline membrane disease. The amniotic fluid can be analyzed by looking for an appropriate number of lamellar bodies. Other tests for fetal lung maturity include: fluorescence polarization (fpol), lecithin:sphingomyelin (LS) ratio, and for phosphatidyl glycerol (PG). These tests have poor positive predictive value for respiratory distress, so the decision to do amniocentesis can be made by consideration of issues around gestational age and urgency of delivery. Risks with amniocentesis are uncommon, but include fetal loss and maternal Rh sensitization. The increased risk for fetal mortality following amniocentesis is about 0.5% above what would normally be expected. Rh negative mothers can be treated with RhoGam. Contamination of fluid from amniocentesis by maternal cells is highly unlikely. If oligohydramnios is present, then amniotic fluid is difficulk to obtain. It is sometimes possible to instill saline into the amniotic cavity and then remove fluid for analysis. Chorionic Villus Sampling (CVS)In this procedure, a catheter is passed via the vagina through the cervix and into the uterus to the developing placenta under ultrasound guidance. An alternative approach is transabdominal. The introduction of the catheter allows sampling of cells from the placental chorionic villi. These cells can then be analyzed by a variety of techniques. The most common test employed on cells obtained by CVS is chromosome analysis to determine the karyotype of the fetus. The cells can also be grown in culture for biochemical or molecular biologic analysis. CVS can be safely performed between 9.5 and 12.5 weeks gestation. CVS has the disadvantage of being an invasive procedure, and it has a small but significant rate of morbidity for the fetus; this loss rate is about 0.5 to 1% higher than for women undergoing amniocentesis. Rarely, CVS can be associated with limb defects in the fetus. The possibility of maternal Rh sensitization is present. There is also the possibility that maternal blood cells in the developing placenta will be sampled instead of fetal cells and confound chromosome analysis. Maternal blood sampling for fetal DNAThis technique makes use of the phenomenon of fetal blood cells gaining access to maternal circulation through the placental villi. Ordinarily, only a very small number of fetal cells or cell free DNA enter the maternal circulation in this fashion (not enough to produce a positive Kleihauer-Betke test for fetal-maternal hemorrhage). The sequencing of maternal plasma cell-free DNA (cfDNA testing) can detect fetal autosomal aneuploidy, but without the risks that invasive procedures inherently have. Fluorescence in-situ hybridization (FISH) is another technique that can be applied to identify particular chromosomes of the fetal cells recovered from maternal blood and diagnose aneuploid conditions such as the trisomies and monosomy X. The problem with this technique is that it is difficult to get large amounts of fetal DNA. There may not be enough to reliably determine anomalies of the fetal karyotype or assay for other abnormalities. Maternal serum alpha-fetoprotein (MSAFP)The developing fetus has two major blood proteins–albumin and alpha-fetoprotein (AFP). Since adults typically have only albumin in their blood, the MSAFP test can be utilized to determine the levels of AFP from the fetus. Ordinarily, only a small amount of AFP gains access to the amniotic fluid and crosses the placenta to maternal blood. However, when there is a fetal defect in the body wall, such as a neural tube defect from failure of part of the embryologic neural tube to close, then there is a means for escape of more AFP into the amniotic fluid. Neural tube defects include anencephaly (failure of closure at the cranial end of the neural tube) and spina bifida (failure of closure at the caudal end of the neural tube). The incidence of such defects is less than 1 per 1000 in the United States. Also, if there is an omphalocele or gastroschisis (both are defects in the fetal abdominal wall), the MSAFP will be higher. In order for the MSAFP test to have the greatest utility, the gestational age must be known with certainty. This is because the amount of MSAFP increasses with gestational age (as the fetal liver size and the amount of AFP produced increase). Also, the race of the mother and presence of gestational diabetes are important to know, because the MSAFP can be affected by these factors. The MSAFP is typically reported as multiples of the median (MoM). The greater the MoM, the more likely a defect is present. The MSAFP has the greatest sensitivity between 16 and 18 weeks gestation, but can still be useful between 15 and 22 weeks gestation. However, the MSAFP can be elevated for a variety of reasons which are not related to fetal neural tube or abdominal wall defects, so this test is not 100% specific. The most common cause for an elevated MSAFP is a wrong estimation of the gestational age of the fetus. Using a combination of MSAFP screening and ultrasonography, almost all cases of anencephaly can be found, and most cases of spina bifida. Neural tube defects can be distinguished from other fetal defects (such as abdominal wall defects) by use of the acetylcholinesterase test performed on amniotic fluid obtained by amniocentesis–if the acetylcholinesterase is elevated along with MSAFP then a neural tube defect is likely. If the acetylcholinesterase is not detectable, then some other fetal defect is suggested. NOTE: Prevention of many neural tube defects can be accomplished by supplementation of the maternal diet with just 4 mg of folic acid per day, but this vitamin supplement must be taken a month before conception and through the first trimester. The MSAFP can also be useful in screening for Down syndrome and other trisomies. The MSAFP tends to be lower when triosmy 21 or other chromosomal abnormalities is present. Maternal serum beta-HCGThis test is most commonly used as a test for pregnancy. Beginning about a week following conception and implantation of the developing embryo into the uterus, the trophoblast will produce enough detectable beta-HCG (the beta subunit of human chorionic gonadotropin) to diagnose pregnancy. Thus, by the time the first menstrual period is missed, the beta-HCG will virtually always be elevated enough in maternal urine to provide a positive pregnancy test. The beta-HCG can also be quantified in serum from maternal blood, and this can be useful early in pregnancy when threatened abortion or ectopic pregnancy is suspected, because the amount of beta-HCG will be lower than expected. Later in pregnancy, in the middle to late second trimester, the beta-HCG can be used in conjunction with the MSAFP to screen for chromosomal abnormalities, and Down syndrome in particular. An elevated beta-HCG coupled with a decreased MSAFP suggests Down syndrome. Very high levels of HCG suggest trophoblastic disease (molar pregnancy). The absence of a fetus on ultrasonography along with an elevated HCG suggests a hydatidiform mole. The HCG level can be used to follow up treatment for molar pregnancy to make sure that no trophoblastic disease, such as a choriocarcinoma, persists. Maternal serum unconjugated estriolThe amount of unconjugated estriol in maternal serum is dependent upon a viable fetus, a properly functioning placenta, and maternal well-being. The substrate for estriol begins as dehydroepiandrosterone (DHEA) produced in the fetus. This is further metabolized in the placenta to estriol. The estriol crosses to the maternal circulation and is excreted by the maternal kidney in urine or by the maternal liver in the bile. The measurement of serial estriol levels in the third trimester will give an indication of general well-being of the fetus. If the estriol level drops, then the fetus is threatened and delivery may be necessary emergently. Estriol tends to be lower when Down syndrome is present or when there is adrenal hypoplasia with anencephaly. Inhibin-ADimeric inhibin-A is secreted by the placenta and by the maternal ovarian corpus luteum. Dimeric inhibin-A can be measured in maternal serum. An increased level of inhibin-A is associated with an increased risk for trisomy 21. A high inhibin-A may also be associated with risk for preterm delivery. Pregnancy-associated plasma protein A (PAPP-A)Low levels of PAPP-A as measured in maternal serum during the first trimester may be associated with fetal chromosomal anomalies including trisomies 13, 18, and 21. In addition, low PAPP-A levels in the first trimester may predict an adverse pregnancy outcome, including a small for gestational age (SGA) baby or stillbirth. A high PAPP-A level may predict a large for gestational age (LGA) baby. “Triple” or “Quadruple” screenCombining the maternal serum assays may aid in increasing the sensitivity and specificity of detection for fetal abnormalities. The classic test is the “triple screen” for alpha-fetoprotein (MSAFP), beta-HCG, and estriol (uE3). The “quadruple screen” adds inhibin-A. Approach to diagnosis of trisomy 21 can be based upon timing. In the first-trimester combined screening with measurement of nuchal translucency, PAPP-A, and beta-HCG has a high diagnostic yield. Second-trimester quadruple screening with measurement of AFP, beta-HCG, unconjugated estriol, and inhibin A has a high diagnostic yield. Both can be combined to provide high rates of detection of trisomy 21. The detection rate of trisomy 21 for the “triple screen” is about 70%, and for the “quad screen” about 80%, with false positive rates of 7% and 6% respectively. Combining the “quad screen” from the second trimester with results of PAPP-A and NT from the first trimester yields a Down syndrome detection rate of 90%, with 3% false positive rate. Without the NT test, combination of the 5 serum tests yields a detection rate for trisomy 21 of 87% with 3.2% false positive rate.
Note: the levels of these analytes may change markedly during pregnancy, so interpretation of the measurements depends greatly upon knowing the proper gestational age. Otherwise, results can be misinterpreted. Rather than absolute values, the test results are typically reported as “multiples of the median” or MoM to adjust for the effect of gestational age, as well as maternal weight and race if applicable. Techniques for Pathologic ExaminationA variety of methods can be employed for analysis of fetal and placental tissues: Gross Examination
Microscopic Examination
Radiography
Microbiologic Culture
Karyotyping
FISH (performed on fresh tissue or paraffin blocks)
DNA Probes
Biochemical Analysis
Flow Cytometry
Electron Microscopy (EM)
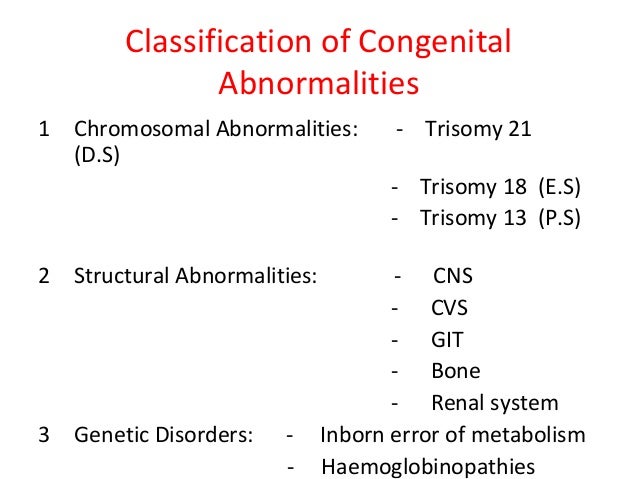
Overview of Fetal-Placental AbnormalitiesChromosomal Abnormalities
Neural Tube Defects
Hydrops Fetalis
Congenital Infections
Disruptions
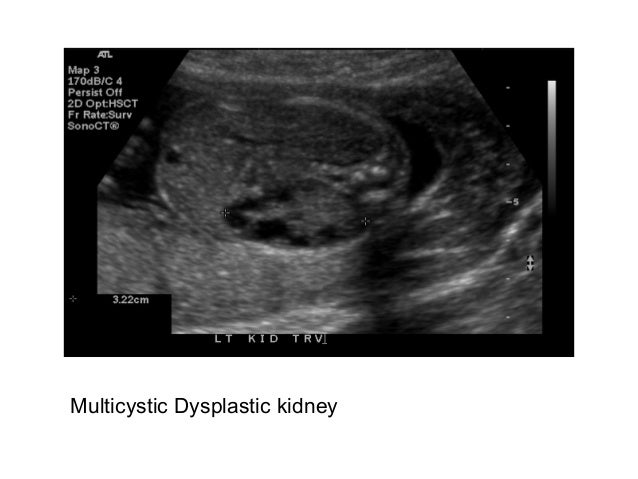
Renal Cystic Disease
Congenital Neoplasms
Skeletal Abnormalities
Placental Abnormalities
|
**************************************************************************************



********************************************************************************

***************************************************************************