Menu
Close
Back
Welcome to
Together is a new resource for anyone affected by pediatric cancer - patients and their parents, family members, and friends.
Learn MoreLiver cancer is rare in children and teens. It accounts for 1–2% of childhood cancers. Types of childhood liver cancers include:
Liver cancer accounts for 1–2% of childhood cancers. Childhood liver cancers include hepatoblastoma, hepatocellular carcinoma, fibrolamellar hepatocellular carcinoma, and undifferentiated embryonal sarcoma of the liver.
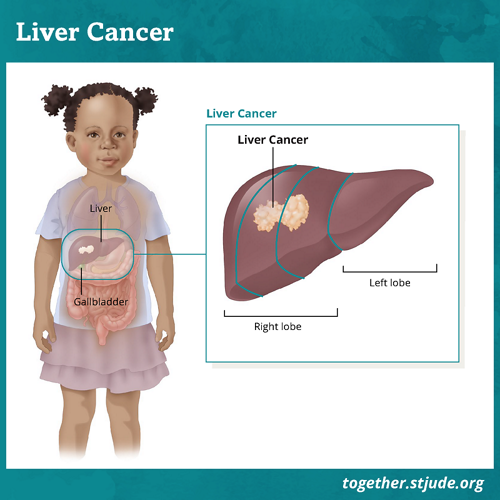
The liver is a large organ on the top right side of the abdomen. The liver:
Liver cancer occurs when cancer cells form tumors in the tissue of the liver.
Surgery is the main treatment option for liver cancers. The goal of surgery is to remove as much of the tumor as possible. Patients have a good chance for cure if the tumor can be completely removed.
Chemotherapy may be used to shrink the tumor before surgery. It can also help stop or slow the growth of cancer cells after surgery.
Survival depends on whether surgery can remove the tumor and whether the cancer has spread beyond the liver.
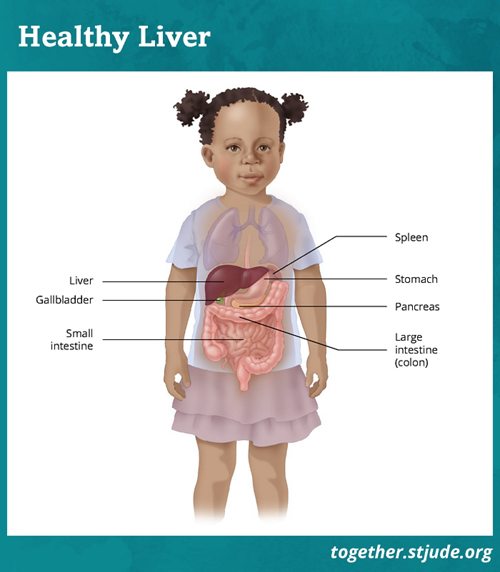
The liver helps clear waste from the blood, makes bile to help digest food, and stores energy to fuel the body.
Symptoms of liver cancer may depend on the size of the tumor and if it has spread beyond the liver. Symptoms of liver cancer include:
Doctors use several types of tests to evaluate liver tumors and make a diagnosis. These tests include:
Doctors often classify liver tumors based on where the cancer is before the patient has treatment. This system is called pretreatment extent of disease (PRETEXT). PRETEXT groups (1, 2, 3, 4) depend on which parts of the liver have cancer.
| PRETEXT Group | Amount of the liver involved |
|---|---|
| PRETEXT Group 1 |
One section of the liver is involved. |
| PRETEXT Group 2 | One or 2 sections of the liver are involved. Two side-by-side sections are free of tumor. |
| PRETEXT Group 3 | Two or 3 sections of the liver are involved. One or 2 sections are free of tumor, but these sections do not touch. |
| PRETEXT Group 4 |
All 4 sections of the liver are involved. |
If the tumor can be completely removed with surgery, the patient has a good chance for cure.
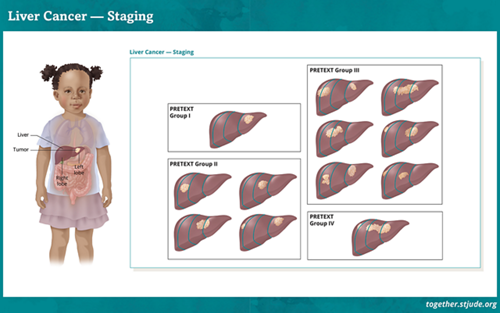
Staging of liver tumors depends on where cancer is found in the liver.
Patients who have a liver transplant need lifelong immunosuppression medication. These drugs keep the body from attacking or rejecting the new liver. Because the medicines lower the body’s natural defenses, patients may have an increased risk for infection. But many people live normal, healthy lives after an organ transplant. It is important to have regular medical care and take medicines as prescribed.
Survivors of childhood liver cancer should have long-term follow-up care. Some treatments can cause late effects. These are health problems that happen months or years after treatment has ended.
For general health and disease prevention, all cancer survivors should adopt healthy lifestyle and eating habits. They should have regular checkups and screenings by primary health care providers. Childhood cancer survivors treated with chemotherapy should be monitored for late effects of therapy. Possible health concerns include hearing loss and kidney problems (cisplatin) and heart problems (anthracylcines).
Your child should receive a survivorship care plan after they complete treatment. It includes guidance on health screenings, disease risk factors, and how to improve health. Survivors should share this plan with their health care providers.
—
Reviewed: December 2022